| Catalog number | RC-CF28 |
| Summary | Detection of anti-Toxoplasma IgG/IgM antibodies within 10 minutes |
| Principle | One-step immunochromatographic assay |
| Detection Targets | Toxoplasma IgG/IgM antibody |
| Sample | Feline Whole Blood, Plasma or Serum |
| Reading time | 10 ~ 15 minutes |
| Sensitivity | IgG : 97.0 % vs. IFA , IgM : 100.0 % vs. IFA |
| Specificity | IgG : 96.0 % vs. IFA , IgM : 98.0 % vs. IFA |
| Quantity | 1 box (kit) = 10 devices (Individual packing) |
| Contents | Test kit, Buffer bottle, and Disposable droppers |
| Storage | Room Temperature (at 2 ~ 30℃) |
| Expiration | 24 months after manufacturing |
| Caution | Use within 10 minutes after openingUse appropriate amount of sample (0.01 ml of a dropper) Use after 15~30 minutes at RT if they are stored under cold circumstances Consider the test results as invalid after 10 minutes |
Cats are the only primary hosts of T.gondii; they are the only mammals in which Toxoplasma is passed through the feces. In the cat, the reproductive form of T.gondii lives in the intestine and the oocysts (egg-like immature forms) exit the body in the feces. The oocysts must be in the environment 1-5 days before they are infective. Cats only pass T.gondii in their feces for a few weeks after becoming infected. The oocysts can survive several years in the environment and are resistant to most disinfectants.
The oocysts are ingested by intermediate hosts such as rodents and birds, or other animals such as dogs and humans, and migrate to the muscle and brain. When a cat eats an infected intermediate prey (or part of a larger animal, e.g., a pig), the parasite is released in the cat’s intestine and the life cycle can be repeated
The most common symptoms of toxoplasmosis include fever, loss of appetite, and lethargy. Other symptoms may occur depending on whether the infection is acute or chronic, and where the parasite is found in the body. In the lungs, T.gondii infection can lead to pneumonia, which will cause respiratory distress of gradually increasing severity. Toxoplasmosis can also affect the eyes and central nervous system, producing inflammation of the retina or anterior ocular chamber, abnormal pupil size and responsiveness to light, blindness, incoordination, heightened sensitivity to touch, personality changes, circling, head pressing, twitching of the ears, difficulty in chewing and swallowing food, seizures, and loss of control over urination and defecation.Toxoplasmosis is usually diagnosed based on the history, signs of illness, and the results of supportive laboratory tests. Measurement of IgG and IgM antibodies to Toxoplasma gondii in the blood can help diagnose toxoplasmosis. The presence of significant IgG antibodies to T.gondii in a healthy cat suggests that the cat has been previously infected and now is most likely immune and not excreting oocysts. The presence of significant IgM antibodies to T.gondii, however, suggests an active infection of the cat. The absence of T.gondii antibodies of both types in a healthy cat suggests that the cat is susceptible to infection and thus would shed oocysts for one to two weeks following infection.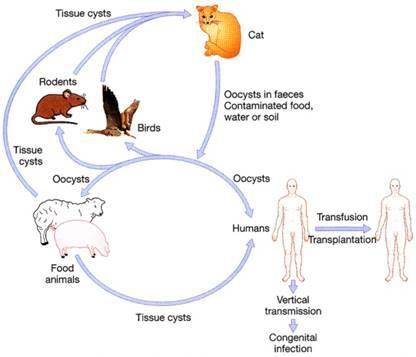 Toxoplasmosis is a disease caused by a single celled parasite called Toxoplasma gondii (T.gondii). Toxoplasmosis is one of the most common parasitic diseases and has been found in nearly all warm-blooded animals, including pets and humans. Cats are important in the epidemiology of T. gondii because they are the only hosts that can excrete environmentally resistant oocysts. Most cats infected with T.gondii will not show any symptoms. Occasionally, however, clinical disease toxoplasmosis occurs. When disease does occur, it may develop when the cat’s immune response is not adequate to stop the spread of tachyzoite forms. The disease is more likely to occur in cats with suppressed immune systems, including young kittens and cats with feline leukemia virus (FELV) or feline immunodeficiency virus (FIV).
Toxoplasmosis is a disease caused by a single celled parasite called Toxoplasma gondii (T.gondii). Toxoplasmosis is one of the most common parasitic diseases and has been found in nearly all warm-blooded animals, including pets and humans. Cats are important in the epidemiology of T. gondii because they are the only hosts that can excrete environmentally resistant oocysts. Most cats infected with T.gondii will not show any symptoms. Occasionally, however, clinical disease toxoplasmosis occurs. When disease does occur, it may develop when the cat’s immune response is not adequate to stop the spread of tachyzoite forms. The disease is more likely to occur in cats with suppressed immune systems, including young kittens and cats with feline leukemia virus (FELV) or feline immunodeficiency virus (FIV).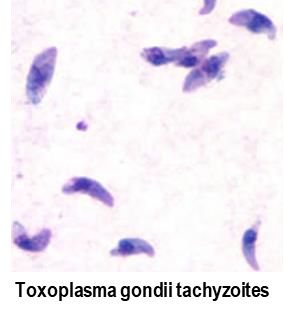 No vaccine is as yet available to prevent either T.gondii infection or toxoplasmosis in cats, humans, or other species. Therefore, treatment usually involves a course of an antibiotic called clindamycin. Other drugs that are used include pyrimethamine and sulfadiazine, which act together to inhibit T.gondii reproduction. Treatment must be started as soon as possible after diagnosis and continued for several days after signs have disappeared.Acute infection is characterized by a prompt rise in IgM antibody, followed in 3-4 weeks by a rise in IgG class antibody. IgM antibody levels peak approximately 3-4 weeks post onset of symptoms and remain detectable for 2-4 months. IgG class antibody peaks in 7-12 weeks, but declines much more slowly than IgM antibody levels and remains elevated for over 9-12 months.
No vaccine is as yet available to prevent either T.gondii infection or toxoplasmosis in cats, humans, or other species. Therefore, treatment usually involves a course of an antibiotic called clindamycin. Other drugs that are used include pyrimethamine and sulfadiazine, which act together to inhibit T.gondii reproduction. Treatment must be started as soon as possible after diagnosis and continued for several days after signs have disappeared.Acute infection is characterized by a prompt rise in IgM antibody, followed in 3-4 weeks by a rise in IgG class antibody. IgM antibody levels peak approximately 3-4 weeks post onset of symptoms and remain detectable for 2-4 months. IgG class antibody peaks in 7-12 weeks, but declines much more slowly than IgM antibody levels and remains elevated for over 9-12 months.